Do Kids Outgrow ADHD? Understanding Symptom Changes Over Time

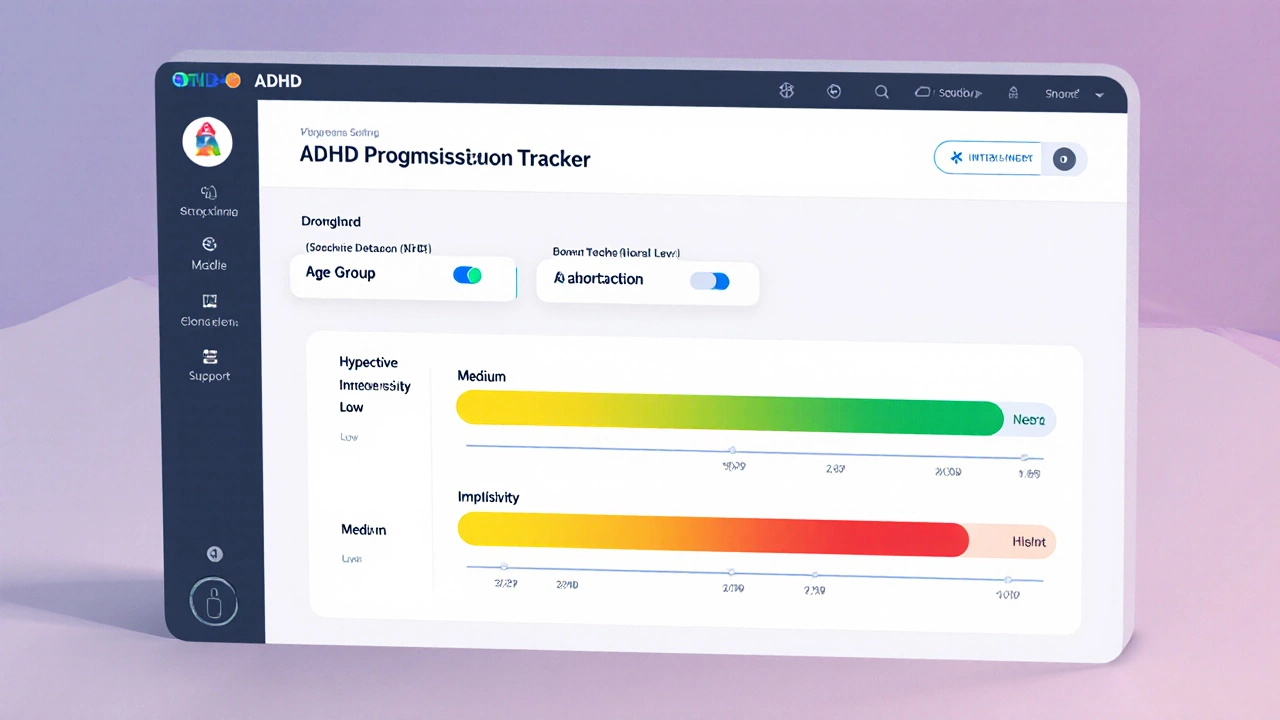
ADHD Symptom Progression Tracker
This interactive tracker shows how ADHD symptoms typically evolve across different life stages. Adjust the sliders to see how different factors influence symptom improvement.
Based on current settings, this age group typically shows a moderate improvement in symptoms with adequate support. About 45% of individuals continue to meet full criteria for ADHD into adulthood.
Did You Know?
About 30-40% of children with ADHD see a significant reduction in core symptoms by late teens, but symptoms often persist into adulthood. Early intervention and ongoing support significantly impact long-term outcomes.
Key Takeaways
- About 30‑40% of children with ADHD see a significant reduction in core symptoms by late teens.
- Improvement is linked to brain maturation, supportive environments, and early treatment.
- Some retain symptoms into adulthood; ongoing support can still lead to successful outcomes.
- Watch for specific behavioral signs that indicate real progress versus temporary coping.
- Regular check‑ins with clinicians, schools, and families are essential for a smooth transition.
When we talk about ADHD (Attention‑Deficit/Hyperactivity Disorder, a neurodevelopmental condition marked by inattention, hyperactivity, and impulsivity), the big question many parents ask is whether their kids will simply “outgrow” it. The answer isn’t a straight yes or no-it’s a mix of biology, environment, and timely help. Below we break down what the research says, why some kids improve, and how you can support a child at every stage.
What Does “Outgrow” Really Mean?
Outgrowing ADHD isn’t about magically losing a label. It means the core symptoms-trouble focusing, excess activity, and impulsive actions-become mild enough that they no longer interfere with school, relationships, or daily life. Many children still retain the diagnosis on paper but function at a level comparable to peers.
How Common Is Symptom Remission?
Long‑term studies tracking kids from elementary school into their twenties show a wide range of outcomes. A 2023 longitudinal cohort of 1,200 participants found:
- 33% showed significant remission of hyperactivity and impulsivity by age 18.
- 45% continued to meet full criteria for ADHD into adulthood.
- 22% had partial remission-symptoms persisted but were manageable with coping strategies.
These numbers tell us that while a good chunk of children improve, a majority still need some form of support past teenage years.
Factors That Influence Persistence or Remission
Several key elements shape whether ADHD symptoms fade, stay the same, or worsen:
- Genetics: Family studies estimate heritability at 70‑80%, so a strong genetic load can keep symptoms alive.
- Brain Development: The prefrontal cortex, responsible for planning and impulse control, continues maturing into the mid‑20s. Faster maturation often aligns with symptom drop‑off.
- Environmental Support: Structured routines, positive school policies, and engaged parents boost adaptive coping.
- Gender: Girls are more likely to present inattentive symptoms, which sometimes get missed early, leading to later recognition and different trajectories.
- Comorbidities: Co‑occurring anxiety, learning disabilities, or sleep issues can hinder remission.
Typical Trajectory: Childhood → Teen → Adult
Think of ADHD as a moving target. Here’s a rough timeline based on large‑scale data:
- Early Childhood (6‑10): Hyperactivity peaks, inattention shows up in classroom settings.
- Middle Adolescence (11‑15): Impulsivity may decline as hormones shift, but academic demands rise, exposing lingering inattentive traits.
- Late Teens (16‑19): Around one‑third experience marked symptom reduction; others stabilize at a moderate level.
- Early Adulthood (20‑25): Those whose prefrontal cortex has fully matured often see the biggest drop in hyperactivity; inattention may persist but becomes manageable.
It’s not a one‑size‑fits‑all path, but the pattern helps parents anticipate where challenges may pop up.
Signs That Symptoms Are Improving
Rather than relying on checklists, watch for real‑world changes:
- Spontaneous organization-child starts using a planner without prompting.
- Reduced need for external reminders; they finish homework with minimal supervision.
- Better peer relationships-fewer conflicts and more sustained play.
- Consistent sleep patterns and less daytime fatigue.
- Self‑advocacy-recognizing when they’re distracted and taking steps to refocus.
If you notice these trends over several months, it likely signals genuine progress rather than a temporary fix.
When Symptoms Stay Strong: Need for Ongoing Support
For the 45% who keep meeting full ADHD criteria into adulthood, continued help makes a huge difference. Two main avenues dominate:
- Medication: Stimulants (like methylphenidate) and non‑stimulants (like atomoxetine) remain effective for many, especially when combined with behavioral strategies.
- Behavioral Therapy: Cognitive‑behavioral approaches teach planning, time‑management, and emotional regulation skills.
Even if a child seems to have “outgrown” hyperactivity, inattentive symptoms can still affect college, work, and relationships. A flexible, long‑term plan keeps them on track.
Practical Steps for Parents
- Schedule regular diagnostic reviews with a pediatric psychologist or psychiatrist-aim for at least once a year during school years.
- Create a visual schedule at home; simple charts help kids internalize routines.
- Partner with teachers: request classroom accommodations (e.g., extended test time, seat near the teacher).
- Encourage physical activity-sports, structured play, or even daily walks boost executive function.
- Monitor sleep hygiene: consistent bedtime, limited screen time, and a calm pre‑sleep routine reduce inattentiveness.
- Consider a trial of medication under professional guidance if academic or social performance stalls.
- Model coping strategies: talk out loud about how you break big tasks into small steps.
Remember, you don’t have to navigate this alone. Support groups, online forums, and local ADHD workshops can provide fresh ideas and emotional relief.
Comparison Table: Symptom Persistence by Age Group
| Age Range | Hyperactivity | Inattention | Impulsivity | Typical % Still Meeting Full Criteria |
|---|---|---|---|---|
| 6‑10 | High | Moderate | High | ≈ 80% |
| 11‑15 | Medium (declines) | Medium‑High | Medium | ≈ 65% |
| 16‑19 | Low | Medium | Low‑Medium | ≈ 45% |
| 20‑25 | Very Low | Low‑Medium | Low | ≈ 30‑35% |

Frequently Asked Questions
Can a child stop taking medication if symptoms improve?
Yes, but only under a doctor’s guidance. A gradual taper lets the clinician watch for any rebound in attention or behavior problems. Many families choose to keep a low dose during school years and pause over summer.
Is it normal for ADHD to appear only in adulthood?
True adult‑onset ADHD is rare. Most adults who get diagnosed had early‑life symptoms that were never formally identified. Retrospective assessments often reveal childhood signs.
Do girls outgrow ADHD less often than boys?
Research shows girls are more likely to retain inattentive symptoms, partly because they’re less likely to receive early diagnosis and intervention. Early support can narrow this gap.
How can schools help a teen who’s still struggling?
Accommodations like extended test time, preferential seating, and breaking assignments into chunks are proven to boost performance. A 504 or IEP plan formalizes these supports.
What lifestyle habits aid long‑term remission?
Regular aerobic exercise, consistent sleep, balanced nutrition, and mindfulness practices improve executive function and reduce stress, all of which help keep symptoms in check.
Bottom line: ADHD isn’t a simple “outgrow it” story, but many children do see a real fade‑out of the most disruptive symptoms. Understanding the factors, watching for genuine progress, and staying proactive with support will give your child the best chance at thriving at every age.

