How Long Should You Wait to Pump After Birth?

Pumping Timeline Calculator
Your Personalized Timeline
Next Steps
- Store milk properly: Room temp (4h), Fridge (4d), Freezer (6-12m)
- Consult lactation professional if no milk after 48h pumping
- Focus on baby-led feeding for healthy milk supply
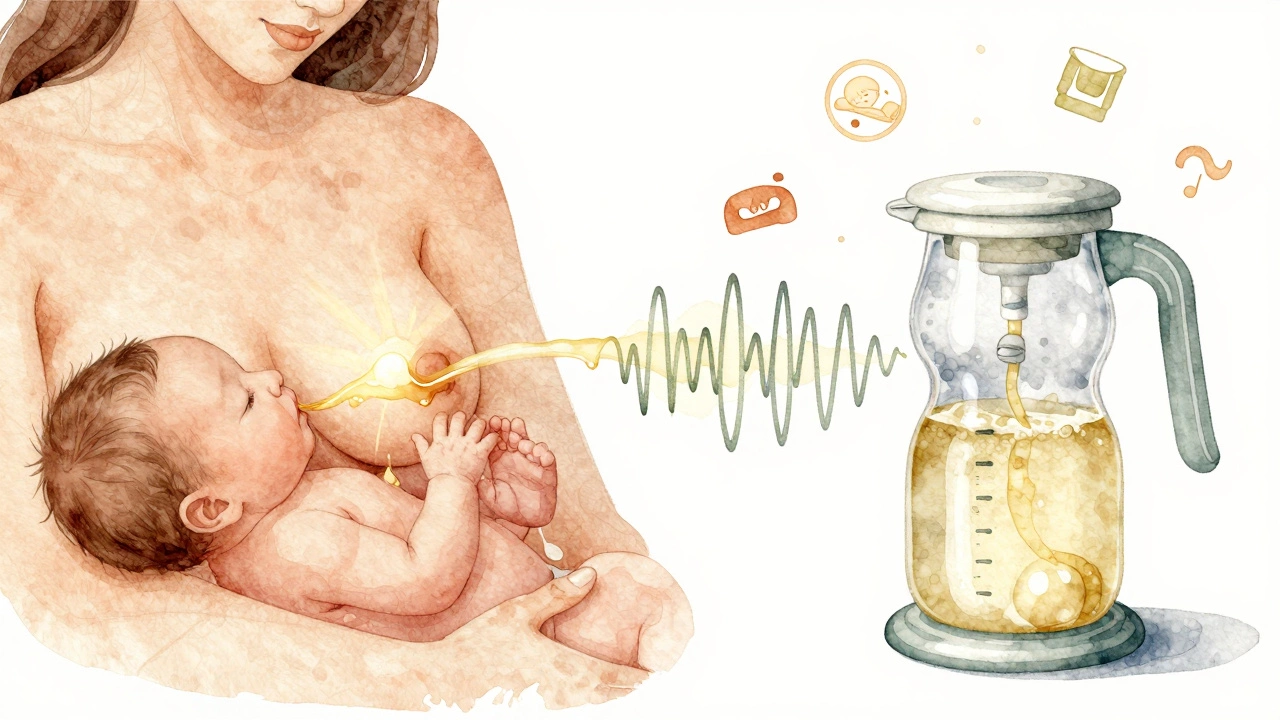
After giving birth, your body starts making milk-but when should you actually start pumping? Many new parents feel pressure to get the pump out right away, but waiting a little longer can make a big difference in how well your milk supply establishes. The truth is, there’s no single right time, but there are clear guidelines based on what your body needs and what your baby needs.
Wait at least 24 to 48 hours if your baby is feeding well
If your baby is latching well and feeding every 2 to 3 hours, you don’t need to pump in the first 24 to 48 hours after birth. Your body is producing colostrum-thick, golden, nutrient-packed fluid that’s perfect for your newborn. It’s not a lot, but it’s enough. Pumping too early can confuse your body. It doesn’t need to make more milk yet. Your baby’s stomach is the size of a marble. You don’t need a gallon of milk.
Studies from the American Academy of Pediatrics show that mothers who delay pumping for the first 48 hours, as long as breastfeeding is going well, have better long-term milk supply. Why? Because early pumping can trigger a signal that you’re not feeding enough, leading your body to overproduce or underproduce, depending on how often you pump. Let your baby set the pace. Their suck is the most effective way to tell your body how much milk to make.
Start pumping if your baby can’t feed directly
If your baby is in the NICU, has a tongue tie, is premature, or is too sleepy to latch, then you need to start pumping sooner. In these cases, begin within 6 hours after birth if possible. The first milk you express is colostrum, and even a teaspoon at a time is valuable. Hospitals often provide hospital-grade pumps for this reason. Don’t wait for your milk to "come in"-you’re not waiting for volume, you’re building the foundation.
One mother in Vancouver shared that she pumped every 2 to 3 hours starting 5 hours after her twins were born. She didn’t get much at first-sometimes just 5 milliliters per session-but by day three, she was producing enough to freeze and feed them by bottle. Consistency mattered more than quantity.
Don’t pump to "build up" a stash before leaving the hospital
Many new parents think they need to start pumping right away to stockpile milk. That’s not necessary. Your body doesn’t store milk like a fridge. It makes what’s needed, when it’s needed. Pumping for a stash in the first 48 hours can lead to oversupply, engorgement, or even mastitis. You’ll feel overwhelmed, sore, and possibly guilty if you don’t fill a dozen bags.
Instead, focus on skin-to-skin contact, frequent feeding, and rest. Your milk will come in around day 3 or 4. That’s when you’ll notice your breasts feel fuller. That’s the signal your body is shifting from colostrum to mature milk. Only then should you consider pumping to build a reserve-unless your baby needs it.
When you do start pumping, how often and how long?
If you’re pumping because your baby isn’t feeding directly, aim for 8 to 12 sessions in 24 hours. That’s about every 2 to 3 hours, including overnight. This mimics how a newborn feeds. Each session should last 15 to 20 minutes per breast, even if you don’t see much coming out. The stimulation is what matters.
Use a double electric pump if you can. It saves time and increases prolactin, the hormone that boosts milk production. A single pump might take 40 minutes for both breasts. A double pump cuts that to 20. That’s a big difference when you’re sleep-deprived.
Don’t worry if you’re only getting 1 to 2 ounces per session in the first few days. That’s normal. By day 5, most mothers are producing 15 to 30 ounces total per day. That’s enough for a full-time bottle-feeding schedule.

Signs you’re pumping too soon or too much
Here’s what to watch for:
- Your breasts feel rock hard and painful (engorgement)
- You’re getting fewer ounces than you started with after a few days
- You feel exhausted or anxious every time you pump
- Your baby is fussy, gassy, or spitting up more than usual
These are signs your body is being overstimulated. If you’re pumping because you think you should, not because your baby needs it, cut back. Let your baby lead. If you’re unsure, talk to a lactation consultant. Most hospitals offer free support for the first week after discharge.
What if you’re going back to work?
If you plan to return to work or need to be away from your baby for long stretches, start practicing pumping 2 to 3 weeks before your return. That gives you time to build a small freezer stash and get used to the routine. But don’t start before your milk comes in. Trying to pump before day 3 or 4 just leads to frustration.
One working mom in Burnaby started pumping once a day at 10 days postpartum. She didn’t aim for a full day’s supply right away. She just wanted to get comfortable with the pump, understand her output, and test different bottles. By day 14, she had 12 ounces frozen. She didn’t stress about the rest. She trusted her body.
It’s okay if you don’t pump at all
Some parents never pump. That’s fine. If your baby is feeding well and gaining weight, you don’t need to pump. Pumping isn’t a measure of success. Breastfeeding is. Bottle-feeding expressed milk is just one option. Many families use formula, donor milk, or a combination. Your worth as a parent isn’t tied to how much milk you express.
What matters is that your baby is fed, held, and loved. Whether that happens at the breast, the bottle, or both, it’s all valid.
What kind of pump should you use?
Not all pumps are created equal. For occasional use, a basic single electric pump works fine. But if you’ll be pumping regularly, invest in a hospital-grade double pump. Brands like Medela, Spectra, and Hygeia are trusted by hospitals and moms alike. Look for features like adjustable suction, memory settings, and quiet operation.
Insurance often covers a pump under the Affordable Care Act. Call your provider. You might get one for free-or close to it.
How to store pumped milk safely
Once you start pumping, you’ll need to store your milk properly:
- At room temperature (up to 4 hours)
- In the fridge (up to 4 days)
- In the freezer (up to 6 months in a regular freezer, up to 12 months in a deep freezer)
Always label containers with the date and time. Use the oldest milk first. Don’t mix warm milk with cold milk-cool it down first. And never reheat milk more than once.
When to call for help
Reach out to a lactation consultant if:
- You’re not seeing any milk after 48 hours of frequent pumping
- Your breasts are red, hot, or swollen with fever
- Your baby isn’t having 6 wet diapers a day by day 5
- You feel overwhelming sadness, anxiety, or guilt about pumping or feeding
These aren’t signs you’re failing. They’re signs you need support. You’re not alone. Most mothers need help at some point. Asking for it is part of being a good parent.